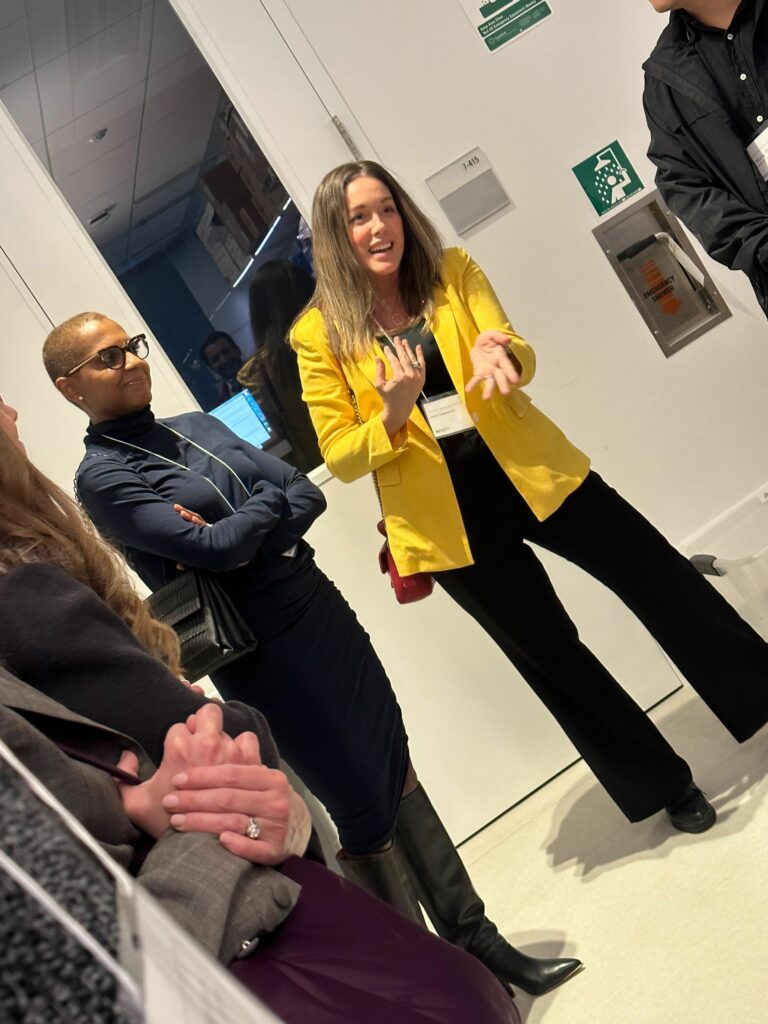
A group of LCRF supporters and staff members were treated to a lab tour and presentation at Northwestern University’s Robert H. Lurie Comprehensive Cancer Center / Feinberg School of Medicine this week.
Leading the tour were Jyoti Patel, MD, who serves on LCRF’s Education + Engagement Committee; Lillian Eichner, PhD; Lu Wang, PhD; 2019 LCRF grantee Nisha Mohindra, MD; and 2013 & 2014 LCRF grantee Mohamed Abazeed, MD, PhD.
Guests and members of LCRF’s staff were treated to lab tours, a brief overview of LCRF-funded research by Northwestern scientists, and a panel of researchers answering attendees’ questions.
Dr. Leon Patanias and Dr. Patel opened the session by thanking all the attendees for their support and emphasizing how it takes partnership between scientists, physicians, and philanthropists to tackle the very difficult task of combating lung cancer. The advances made in lung cancer treatments in the last 15 years have been exponential – just 15 years ago, immunotherapy was an idea that they weren’t sure would work, and now it is standard of care for some lung cancer patients. The advancement of technology has allowed for faster, more efficient data analysis and the ability to use computational models to test hypotheses. Because of the unique collaborations between scientists, patients, advocacy groups, academia and philanthropists, survivorship has increased, toxicity has decreased, and prevention is a real possibility in lung cancer.
Science in action
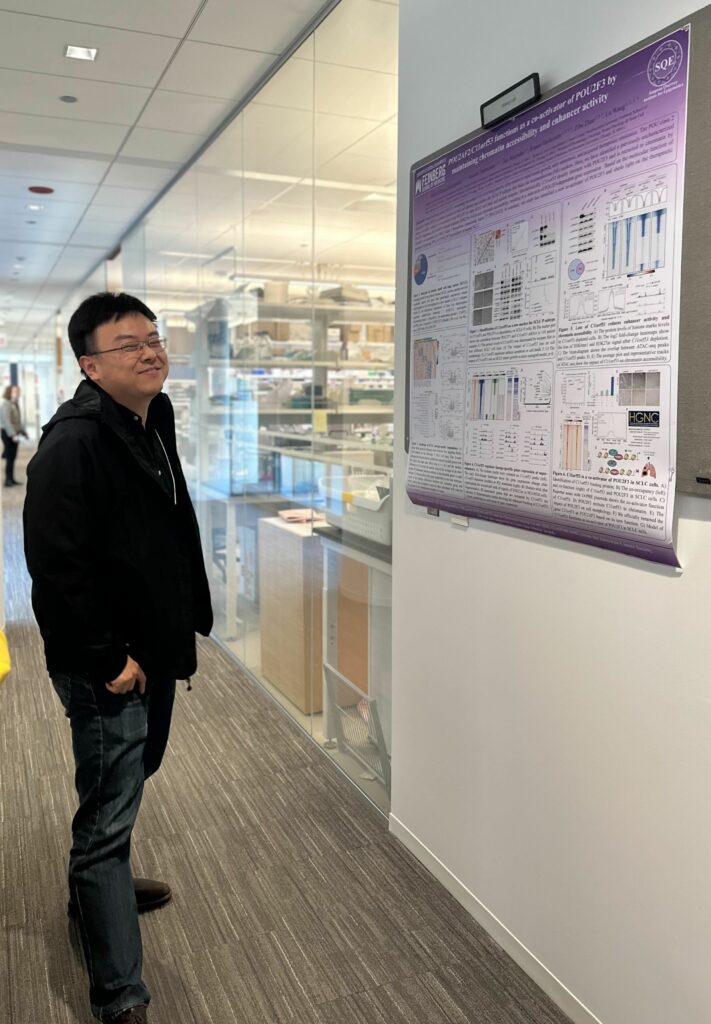
The attendees then broke into two groups to visit two labs: Dr. Wang’s lab, where the focus is on understanding the genetic and epigenetic makeup of small cell lung cancer; and Dr. Eichner’s lab, where the focus is on LKB1 (STK11) which is among the most frequently mutated genes in non-small cell lung cancer (NSCLC), where it is inactivated in ~20% of cases.
Dr. Wang’s lab has recently identified several subtypes of small cell lung cancer, with 347 essential factors that drive this cancer. They have recently discovered, and named, a new gene driving small cell lung cancer and they are now working to better understand its function in the disease. Small cell lung cancer is particularly challenging because its epigenetic makeup shifts in response to whatever treatment the patient is receiving to bypass its effects, making it more difficult to treat. It is also more difficult to detect early, more aggressive and tissue samples are typically too small to test extensively. Stigma plays a large part in obtaining research funding, as 98% of all small cell lung cancers are directly attributed to tobacco use. While Dr. Wang’s lab has made incredible strides in identifying and understanding the many facets of small cell lung cancer, this is still a huge area of unmet need in research.
Research presentation
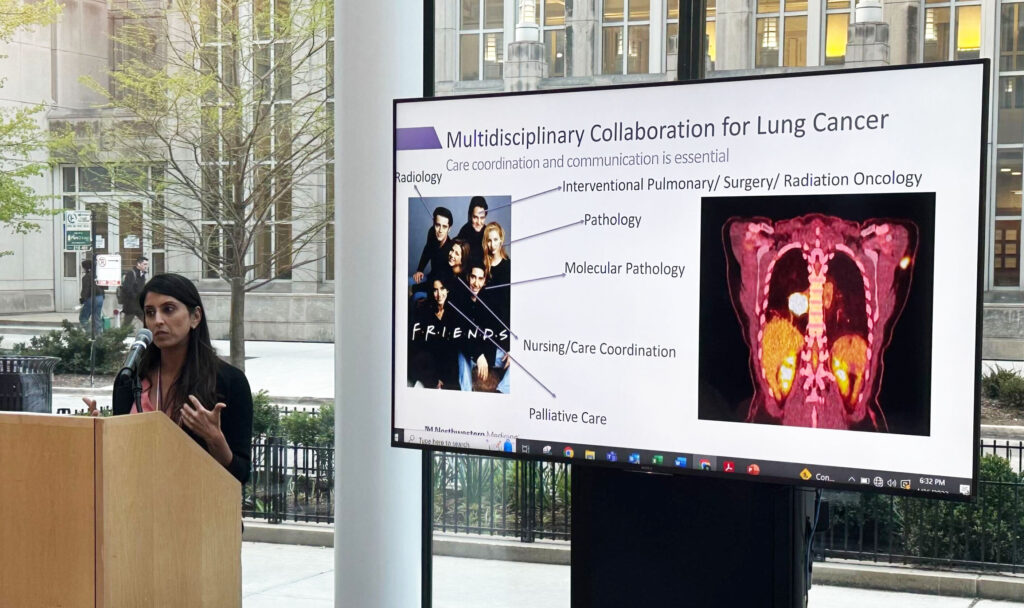
The group then convened for a research presentation by Dr. Mohindra about her work in developing the Patient Level Learning Health System, that coordinates the patient’s treatment regimen with their needs, their experiences, and their feedback and integrates it directly into their medical record where their care team is able to access, address and improve the patient experience. It is an online system that allows patients to see what they are able to self-manage versus what they may need to bring to their doctor.
Dr. Abazeed shared his experiences as a researcher and clinician, bridging the gap through collaboration between basic and translational science. He, too, emphasized the importance of developing resources and tools that remove the “noise” and allow for the researchers to hone in on the findings that will actually have impact for patients in the clinic.
Following the presentations, Drs. Eichner, Wang, Abazeed and Mohindra led a general question and answer session, largely around what the researchers see as the most exciting advancements in lung cancer. Dr. Eichner put it best when she said, “Based on the trajectory of advancements over the last decade, tomorrow is going to be exponentially ahead of yesterday.”
Watch our calendar for future opportunities to see research in action.
Here are some scenes from the event. (Click to enlarge.)