The FDA has approved mobocertinib for the treatment of adult patients with locally advanced or metastatic non–small cell lung cancer with EGFR exon 20 insertion mutations whose disease has progressed on or after platinum-based chemotherapy. Mobocertinib is the first and only oral therapy specifically designed to target EGFR exon 20 insertions.
Read more
FDA approves first targeted therapy for KRAS+ NSCLC
Posted June 1, 2021
The FDA approved Lumakras™ (sotorasib) as the first treatment for non-small cell lung cancer (NSCLC) patients whose tumors have the KRAS G12C genetic mutation and who have received at least one prior systemic therapy. This is the first approved targeted therapy for tumors with any KRAS mutation, which accounts for approximately 25% of mutations in NSCLC.
Read more
Rybrevant approved for NSCLC with EGFR Exon 20 insertion mutations
Posted May 27, 2021
The FDA has approved Rybrevant (amivantamab-vmjw) for adults with non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 20 insertion mutations.
The Guardant360 CDx (Guardant Health Inc.) liquid biopsy test was also approved as a companion diagnostic for use with Rybrevant.
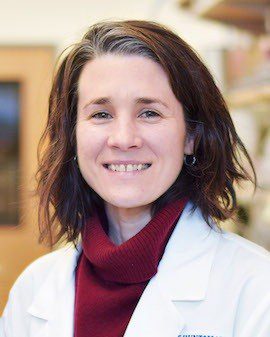
“For the first time, patients with non-small cell lung cancer with EGFR exon 20 insertion mutations will have a targeted treatment option,” said Julia Beaver, M.D., chief of medical oncology in the FDA’s Oncology Center of Excellence and acting deputy director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
Read more
FDA grants fast track status for targeted treatment poziotinib
Posted March 15, 2021
The FDA has granted fast track status for the targeted treatment poziotinib, which is used to treat patients with non-small cell lung cancer (NSCLC) HER2 exon 20 mutations. Fast track is a process intended to accelerate the review of drugs to treat serious conditions and fill an unmet medical need. This new status for poziotinib is welcome news as no FDA approved targeted treatments currently exist for those with the specific HER2 exon 20 mutation.
Read more
Research shows brigatinib provides improved health outcomes
Posted March 9, 2021
Almost a year ago, the FDA approved brigatinib (Alunbrig®) for the first-line of treatment of patients with ALK+ metastatic non-small cell lung cancer (NSCLC). Since then, research has continued to provide evidence that brigatinib has consistent superiority in progression-free survival (PFS) compared to the targeted treatment crizotinib (Xalkori®).
Read more
Lorlatinib approved as targeted therapy for NSCLC
Posted March 8, 2021
Lorlatinib (Lorbrena®) is a targeted treatment that can now be used for metastatic NSCLC patients with ALK-positive tumors in the first-line setting. Prior to this approval, lorlatinib was only approved for use in the second- or third-line setting. The FDA also approved the treatment Ventana ALK (D5F3) CDx Assay as a companion treatment for those using lorlatinib.
Read more
Two promising KRAS inhibitors soon to be FDA approved
Posted February 26, 2021
The KRAS G12C mutation leads to a specific type of lung cancer, in individuals who are likely to have been smokers and likely to respond to immunotherapy. Currently, we have several KRASG12C inhibitors that are under clinical development and may reveal an effective targeted treatments for KRAS G12C patients. Sotorasib (AMG 510) and adagrasib (MRTX849) have shown be to effective and researchers believe that these two treatments are very likely to be approved by the FDA within a year as a second-line treatment. This is positive news that will benefit many KRAS patients through their treatment journey.
Read more
FDA approves immunotherapy for NSCLC patients
Posted February 22, 2021
Yet another immunotherapy is now approved for non- small cell lung cancer (NSCLC) patients! Libtayo® (also known as cemiplimab-rwlc) is an immunotherapy drug that can be used in the first-line setting for NSCLC patients who are not otherwise eligible for surgery or chemoradiation treatment for their diagnosis. NSCLC patients must exhibit high PD-L1 expression with no presence of the EGFR, ALK, or ROS1 aberrations, to be eligible for this new treatment approval.
Read more
FDA approves Cosela to reduce bone marrow suppression in SCLC patients
Posted February 16, 2021
The FDA has granted approval to the first-in-class agent trilaciclib (Cosela™) for the treatment of patients with extensive-stage small cell lung cancer (SCLC) to reduce chemotherapy-induced bone marrow suppression.
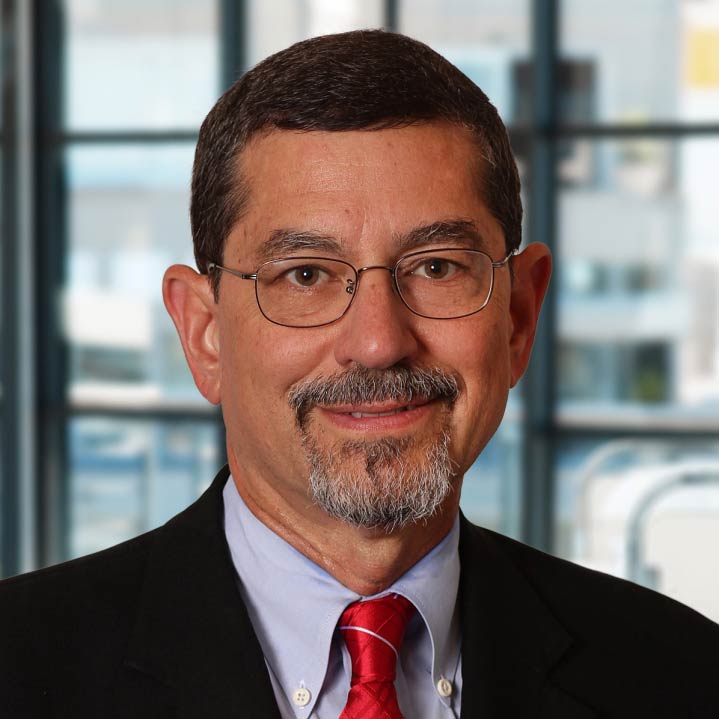
“For patients with extensive-stage small cell lung cancer, protecting bone marrow function may help make their chemotherapy safer and allow them to complete their course of treatment on time and according to plan,” said Albert Deisseroth, MD, PhD, supervisory medical officer in the Division of Non-Malignant Hematology in the FDA’s Center for Drug Evaluation and Research. The approval “will give patients a treatment option that can reduce the occurrence of a common, harmful side effect of chemotherapy.”
Read more
FDA approves Tepmetko for MET exon 14 NSCLC patients
Posted February 4, 2021
On February 3, 2021, the Food and Drug Administration (FDA) granted accelerated approval for tepotinib (Tepmetko®) for the treatment of metastatic non-small cell lung cancer (NSCLC) patients who have the MET exon 14 skipping alterations. This is the second targeted treatment now available for this specific patient group. The FDA approval was based off the VISION trial showing overall response rate was sustained for a median of 10-11 months.
Read more
Trial fails to show benefit to combining EGFR tyrosine kinase inhibitor and anti-VEGF agent
Posted February 3, 2021
In a new clinical trial performed by JAMA Oncology, osimertinib (Tagrisso®) plus bevacizumab (Avastin®) failed to demonstrate prolongation of progression-free survival (PFS) compared with osimertinib alone in patients with non-small cell lung cancer (NSCLC). Several other studies are still ongoing and will be looked upon with interest. Additionally, a phase 3 trial of osimertinib with or without bevacizumab is being conducted and can deliver more insight about this treatment.
Read more
FDA grants priority review for lorlatinab as first line treatment for ALK+ NSCLC
Posted February 2, 2021
The FDA has granted a priority review of the supplemental new drug application for the third-generation ALK inhibitor lorlatinib (Lorbrena®) as a first-line treatment for patients with ALK-positive metastatic non–small cell lung cancer (NSCLC). This advancement can speed up availability of the potentially life-changing medicine lorlatinib. The goal date for the completion of the review has been set by the FDA for April 2021.
Read more
FDA grants breakthrough therapy designation to new immunotherapy drug
Posted January 11, 2021
The FDA has granted a breakthrough therapy designation to a promising new immunotherapy drug called tiragolumab that can be used in combination with atezolizumab (Tecentriq®) as a first-line therapy for metastatic non-small cell lung cancer (NSCLC) patients with high PD-L1 expression. NSCLC patients must not have the EGFR or ALK genomic tumor irregularities present.
This breakthrough therapy designation will accelerate the progress of the CITYSCAPE clinical trial to focus event more on the benefits of tiragolumab as a possible chemotherapy-free combination treatment in earlier stages of cancer.
Read more
FDA approves Tagrisso as first adjuvant therapy for earlier stage NSCLC with certain EGFR mutations
Posted January 4, 2021
On December 18, 2020 the FDA approved osimertinib (Tagrisso®) as the first adjuvant therapy that can be used in NSCLC Stage IB-IIIA patients positive for either EGFR exon 19 or exon 21 L858R genetic mutations. Patients must first have undergone resection, or in other words had their tumor removed with surgery, before receiving Tagrisso.
The most exciting part about this approval is that Tagrisso can now be used to treat NSCLC patients in earlier stages as well as late stage. This provides the potential for an earlier and hopefully more curative therapy, which is great news for the nearly 20% of all lung cancer patients who have the EGFR mutation.
Read more
FDA grants sotorasib breakthrough therapy designation
Posted December 9, 2020
As of December 8, 2020, the FDA has granted a breakthrough therapy designation for a drug called sotorasib for the treatment of patients living with non-small cell lung cancer (NSCLC) containing the KRAS G12C mutation. This treatment may be used on NSCLC patients after they are confirmed to have the KRAS G12C mutation through the use of an FDA-approved diagnostic test and following at least one other systemic therapy.
The KRAS genetic mutation is the most commonly occurring mutation in adenocarcinoma NSCLC. Furthermore, the KRAS G12C mutation affects roughly 13% of all adenocarcinoma NSCLC patients. In the United States alone, 25,000 NSCLC patients will be diagnosed with this specific mutation every year.
This breakthrough therapy designation for sotorasib brings the lung cancer community closer to finding the very first targeted therapy that can be used to treat this commonly occurring genetic mutation.
Read more
FDA approves cobas EGFR mutation test v2
Posted November 5, 2020
The Food and Drug Administration approved “cobas EGFR mutation test v2” to identify NSCLC patients eligible for any of the EGFR inhibitor therapies, including those used to treat EGFR exon 19 and L858R deletions, as well as any EGFR therapies to come in the future.
Read more here.
FDA grants priority review to Libtayo®
Posted November 2, 2020
The Food and Drug Administration granted priority review to cemiplimab-rwlc (Libtayo®) for treatment of certain patients with non-small cell lung cancer.
The designation applies to use as first-line therapy for locally advanced or metastatic NSCLC with 50% or greater PD-L1 expression.
Read more here.
FDA approves diagnostic test for NTRK+
Posted October 27, 2020
On October 23, the Food and Drug Administration approved the next-generation sequencing (NGS)-based FoundationOne CDx test as a companion diagnostic to help identify NTRK+ solid tumor patients eligible for larotrectinib.
Read more here.
FDA grants expedited review for Tagrisso® in early-stage lung cancer
Posted October 21, 2020
The Food and Drug Administration has granted its Priority Review designation for AstraZeneca’s Tagrisso® in certain patients with early-stage lung cancer.
These faster reviews, which take six months instead of the standard 10-month timeframe, are reserved for medicines that demonstrate significant improvements in efficacy or safety for serious diseases.
Read more here.
FDA approves drug for patients with NSCLC RET mutation
Posted September 8, 2020
On September 4, the Food and Drug Administration granted accelerated approval of Gavreto™ (pralsetinib) for people with metastatic non-small-cell lung cancer (NSCLC) with the RET mutation.
Gavreto™ inhibits a receptor tyrosine kinase known as RET, which plays a role in cell proliferation. RET gene mutations or fusions can drive cancer growth, and about 1-2% of NSCLC patients are thought to be affected.
This is the second drug approved for patients whose cancers harbor RET mutations. This approval provides oncologists and patients with an additional option for treatment.
Read more here.
FDA grants priority review to tepotinib for NSCLC patients with MET
Posted August 27, 2020
The Food and Drug Administration has given priority review to tepotinib, a soon-to-be targeted therapy for NSCLC patients with the MET exon 14 mutation.
This new drug will be in addition to Tabrecta™, which was previously approved for MET exon 14.
Read more here.
FDA approves first liquid biopsy with NGS technology for EGFR
Posted August 7, 2020
On August 7, the U.S. Food and Drug Administration approved the Guardant360 CDx assay liquid – or blood – biopsy. This biomarker test uses next-generation sequencing (NGS) technology to identify patients with the epidermal growth factor receptor (EGFR) gene in a deadly form of metastatic non-small cell lung cancer (NSCLC). This is the first approval to combine two technologies — NGS and liquid biopsy — in one diagnostic test in order to guide treatment decisions.
Typically, biomarker testing involves a tissue sample from the primary tumor. This biomarker testing will use blood instead, while still utilizing the NGS biomarker testing normally done on tissue samples.
Read more here.